
Welcome! Thank you for choosing St. Anthony Community Hospital.
Orthopaedic surgery can be daunting, but trusted surgeons committed to timely, exceptional medical care means a patient can confidently look ahead to restored health.
That passion guides the Orthopaedic Surgery team at St. Anthony Community Hospital.
The Orthopaedic team, led by John Juliano, MD, Orthopaedic Surgeon and Chief of Surgery, offers patients a range of exemplary surgical skills and a commitment to patients’ optimum health. The team’s surgical expertise is continually sharpened by their passion for the latest treatment techniques and technology.
“Our priority is to get our patients back to resuming activities they love as quickly as possible,” said Dr. Juliano. “Whether that’s playing a sport or going on a daily walk.”
The orthopaedic surgeries performed at St. Anthony Community Hospital range from:
- Traditional hip and knee joint replacements
- Patient-specific CT-guided 3D model shoulder replacements
- Our orthopaedic doctors specialize in a wide variety of:
- Knee
- Shoulder
- Hand
- Foot
- Elbow
- Sports injury surgeries.
The orthopaedic staff takes pride in achieving high patient satisfaction scores. To ensure that these patients receive the best care after surgery, St. Anthony Community Hospital has a dedicated orthopaedic unit that is staffed with highly trained nurses, case managers and rehabilitation staff.
The Sports Medicine and Orthopaedic Team sees a range of cases, from pediatric to geriatric, and giving personalized attention to each of their patients is a top priority. This echoes St. Anthony Community Hospital’s commitment to providing the very best care, right where patients live.
Please utilize our website as a reference for any questions you may have in regards to The Total Joint Replacement Center or call 845.987.5400.
News
How do you know when a sports injury requires medical attention? Maegen Franco, RN, Total Joint Replacement Program Manager, and Hillary Bastone, Director, Rehabilitation Services at our St. Anthony Community Hospital, discuss surgical and nonsurgical treatment options for sports injuries and other conditions of the knees, hips and shoulders during an interview on WTBQ Radio’s “Health Matters.”
Listen to WTBQ Radio’s “Health Matters” with Kenneth Austin, MD, Director of Surgical Service Line Development. He discuss surgeries that are performed at St. Anthony Community Hospital, Bon Secours Community Hospital and Good Samaritan Hospital, members of the Westchester Medical Center Health Network (WMCHealth). They range from orthopedic, vascular, bariatric, cardiac surgery and more.
Listen to Daniel Tomlinson, MD, Director of the Sports Medicine and Shoulder Program at St. Anthony Community Hospital, a member of the Westchester Medical Center Health Network, on WTBQ Radio. He discusses shoulder injuries, treatments and when to consider shoulder surgery.
Success Stories

Donna Hagedorn
Shoulder Replacement Relieves Years of Progressive Pain

A total shoulder replacement is a major decision but the right one for this Orange County grandma. Learn how this surgery changed her life.

Arun Sharma
A Joint Effort

Photo by Ken Gabrielsen
Arun Sharma’s knees used to ache constantly. But thanks to St. Anthony Community Hospital, he’s getting his kicks out of life again.
By Deborah Skolnik
As seen in Advancing Care
When Arun Sharma isn’t running his electrical construction company, you can find him on the golf course or cheering for his favorite sports teams. Given all that, the 55-year-old Hudson Valley resident is always on the go. But recently, a health issue — aching knees — put a damper on his active lifestyle.
“I noticed the pain when I was at the gym, doing exercises that required bending my knees,” Sharma recalls. “My knees also hurt when I sat for a long time and then stood up.” The problem intensified until climbing stairs turned into an uncomfortable chore. It also became painful to visit job sites, a vital part of Sharma’s occupation. Eventually, his knees ached even when they weren’t bent.
Sharma’s primary care physician referred him to an orthopedic surgeon, who ordered X-rays of both knees. “The specialist stated: ‘You have no cartilage in your knees,’” Sharma remembers. This wearing out of cartilage, called knee arthritis, was making the ends of his knee bones rub together, causing pain and swelling around the joint.
The physician administered cortisone shots to the area in an attempt to reduce the discomfort and swelling and injected a gel to act as a lubricant. Neither provided lasting relief. “I felt like I was going to be this way for the rest of my life,” Sharma said.
Straight Answers
The next option to explore was knee replacement surgery. Sharma was referred to John Hardcastle, MD, Director of Total Joint Replacement at St. Anthony Community Hospital, a member of the Westchester Medical Center Health Network (WMCHealth).
From the first visit, Sharma was confident he’d found the right surgeon. Dr. Hardcastle ordered another set of X-rays and concluded that a full knee replacement was needed.
Sharma appreciates how straightforward Dr. Hardcastle is. “Every question I asked, he answered,” he stated. “There was no ‘I’ll let you know later’ or ‘Let me look into that.’ He was up-front with me.” Dr. Hardcastle suggested operating on the left knee first, since it was causing more pain of the two.

Photo by Ken Gabrielsen
A Caring Call
The week before the operation was an anxious time for Sharma. “Was I nervous!” he remembers. “But then, the night before the surgery, the best thing happened: Dr. Hardcastle called and asked how I was feeling. He stayed on the phone with me for about 15 minutes, ensuring me everything was going to be fine.”
Although Sharma marveled at the kindhearted act, Dr. Hardcastle says he reaches out to all his patients shortly before their surgeries. “I was just raised to do to others as you would like done to you,” he says. “If I were going to have surgery, I feel like getting a call from my surgeon the night before would be calming. It also allows me to answer any questions patients might have.”
Two Successful Surgeries
Sharma underwent the replacement of his left knee. The surgery, which took less than two hours, went as planned. While Sharma was sedated, Dr. Hardcastle made an incision in his knee. Next, he trimmed the ends of the damaged bones of the knee joint, then capped them with metal. Lastly, he placed a plastic spacer between them, creating a new joint.
Sharma stayed in the hospital overnight. “The nurses were wonderful. They kept checking on me,” he says. Within days of his discharge, he was working from home, and a month later, he returned to his office. Assisted by physical therapy, he was back on the golf course in no time. The experience was so good, in fact, that he decided to have his right knee replacement shortly after.
By then, St. Anthony Community Hospital was able to offer robotic-assisted knee replacements. “It allows us to be even more precise with our bone cuts to put in the knee replacement,” Dr. Hardcastle shares. With the robot’s help, surgeons can also more precisely adjust the tension of the ligaments, connective tissues that hold the knee together. “Many patients have a better range of motion sooner,” he says. “I believe that robotic-assisted surgery is the future in terms of accuracy and precision.”
It certainly made a difference in Sharma’s recovery. “I needed a walker after both surgeries. With my first surgery, I used it for a week and a half before switching to a cane,” he says. “But with the robotic-assisted surgery, I was able to switch to the cane on the second or third day. Two weeks to the day after surgery, I didn’t need the cane anymore.”
Once he was fully recovered from both knee replacements, Sharma took two golf trips to Florida. “I have nothing but gratitude for Dr. Hardcastle, St. Anthony Community Hospital, my nurses and my physical therapist. They gave me my life back,” he says. “I walk up and down the stairs easily; I’m playing golf again two to three times a week, and I’m not limping on the course.”
Jim McIntyre

.jpg)
Jim McIntyre can now climb mountains without hip pain. Photo by Kenneth Gabrielsen
Minimally invasive hip-replacement surgery allows a retired teacher to resume his super-active life.
As seen in the May 2021 Issue of Advancing Care. | By Laurie Yarnell
Last summer, orthopaedic surgeon John M. Hardcastle, MD,  received a photo of his patient Jim McIntyre atop Mount Yale, a 14,200-foot mountain in Colorado. This was just four months after Dr. Hardcastle replaced the 67-year-old’s right hip at St. Anthony Community Hospital, in Warwick, a member of the Westchester Medical Center Health Network (WMCHealth).
received a photo of his patient Jim McIntyre atop Mount Yale, a 14,200-foot mountain in Colorado. This was just four months after Dr. Hardcastle replaced the 67-year-old’s right hip at St. Anthony Community Hospital, in Warwick, a member of the Westchester Medical Center Health Network (WMCHealth).
McIntyre, a retired teacher, is an active man who hikes mountains, climbs glaciers and skis. In January 2020, the Summitville resident was climbing in Ecuador “pain-free and on all cylinders.” Soon after, however, he started experiencing severe hip pain, which made it difficult for him to even walk. He consulted Dr. Hardcastle, who had been treating him for several years for osteoarthritis and degenerative joint disease. “You’ll know when it’s time to replace your hip,” he had advised McIntyre. That time had come.
“Despite the pandemic,” says Dr. Hardcastle, “Jim was wise not to delay his care; many safeguards had been put into place to ensure patient safety.”
Smaller Incisions, Quicker Recovery
Dr. Hardcastle used a minimally invasive posterior approach for McIntyre’s surgery. Typically an outpatient procedure, it lasts 30 to 60 minutes. “We take out the ball, or femoral head, which no longer has any cartilage, and replace it with a ceramic one,” says Dr. Hardcastle. “We then remove the socket and replace it with a plastic-and-metal one.” Because this approach requires smaller incisions and results in less handling of soft tissue and less damage to muscle than the more traditional approach, it means quicker recovery and less pain.
Immediate Relief
Shortly after waking from the procedure, McIntyre walked down a hallway with a physical therapist and a walker and then up and down a flight of stairs. “I was already in less pain than before I came in,” he recalls. “I felt better than I had in three years.” This surgery typically requires follow-up doctor appointments and six to 12 weeks of physical therapy.
Now, McIntyre is making plans to hike to the Mount Everest base camp in 2022. “I still have so many things I wanted to accomplish, and I was letting the pain stand in my way,” he says. Reflecting on the procedure that got him back to his active lifestyle, he notes, “The staff at St. Anthony Community Hospital was tremendous. Dr. Hardcastle is also an athlete, so he understands how important it is to get back to an active life. He’s a terrific human being and surgeon.”
‘Pain Is a Treatable Condition’
With a population that is living longer and remaining active, the volume of hip-replacement surgery is on the rise but still underutilized, says Dr. Hardcastle. “Oftentimes, people will deal with the pain and think it’s just part of aging,” he adds, “but hip pain is a treatable condition. Anyone with significant hip pain that’s impacting their quality of life and movement should consult their doctor, even if they think they’re not a candidate due to their age or health conditions.”

Harry Knebel Jr.
Finding Freedom From Chronic Shoulder Pain With 3D Imaging
A highly experienced surgeon and advanced 3D imaging technology power a construction professional’s escape from chronic shoulder pain.
By Brandon O’Connor
As seen in the July/August 2019 issue of Advancing Care
Despite enduring pain for almost three years, Harry Knebel Jr., 66, was unsure he wanted to have shoulder replacement surgery. His procedure was scheduled for late November 2018, but in the weeks leading up to it, the Warwick resident was having second thoughts.
Constant pain, difficulty sleeping, trouble getting dressed and other limitations on his daily activities were commonplace. But the notion of a six-week recovery gave him pause.
“I was really depressed until my 18-year-old grandson, Robbie, told me he didn’t like the depression I was in,” Knebel recalls. “That’s when I decided I was going to do it. My mind made a complete 180 – and after that point, I was eager to have it done.”
Unlike knees and hips — weight-bearing joints that wear out frequently — shoulders typically only have to be replaced in people whose lifestyle places extra stress on them. This can include weightlifters, athletes and manual laborers like Knebel, who spent more than 25 years working as a construction contractor.
Emboldened by his grandson and spurred by multiple recommendations, Knebel decided to see Daniel Tomlinson, MD, Director of the Sports Medicine and Shoulder Program at St. Anthony Community Hospital, a member of the Westchester Medical Center Health Network (WMCHealth).
At that appointment, Knebel learned that shoulder replacements are the best option to ease osteoarthritis pain in the shoulder. Knebel held off for a few more months but returned to see Dr. Tomlinson when he could tolerate the pain no longer.
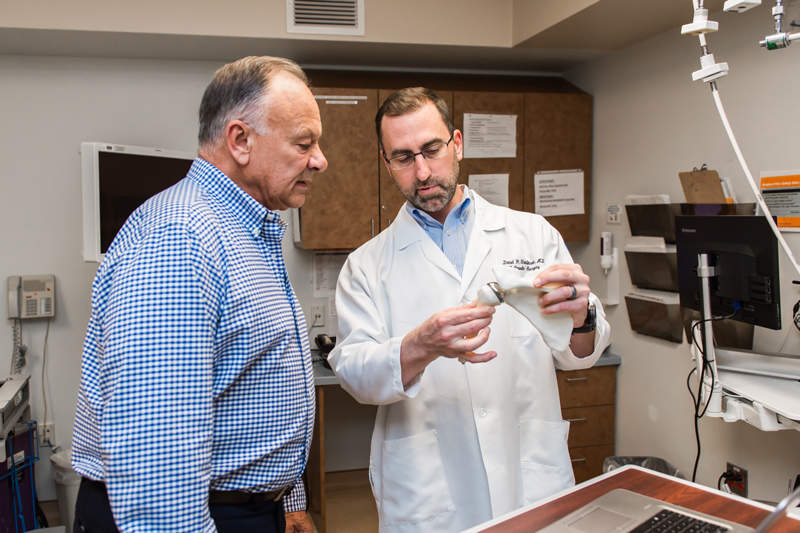
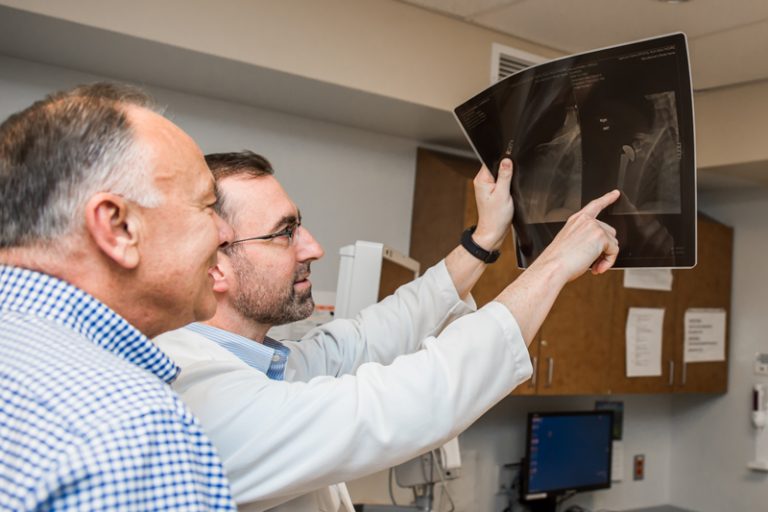
Knebel with Dr. Tomlinson
Dr. Tomlinson performs 80 to 100 of these procedures annually. His extensive experience, coupled with recent technical advancements, have led to continuously improving results for his patients.
“Basically, the goal of any joint replacement is to restore the optimal function of the joint by recreating the patient’s anatomy as close to normal as possible,” Dr. Tomlinson says. “Years ago, shoulder replacements only came in a few different sizes to choose from, so there were a lot of surgeries done that didn’t precisely match the patient’s native anatomy.” Today’s expanded size options, says Dr. Tomlinson, result in implants virtually indistinguishable from the natural joint they replace.
Unlike knee- and hip-replacement joints, which have shorter lifespans due to frequent use, shoulder replacements were more likely to come loose from the shoulder socket.
In recent years, the mechanism for attaching the stem and socket to the bone has improved. However, the biggest advancement has been the improved ability to precisely align the implant.
Placement of a socket even just a few millimeters off can drastically impact shoulder function. Until a few years ago, doctors were forced to partially estimate the placement, because doctors were unable during surgery to see the entire shoulder blade, just the socket. This is because the scapula, or shoulder bone, is covered in soft tissue and muscle. Arthritis also can change the shape of the socket. During surgery, the goal is to recreate the patient’s pre-arthritis anatomy.
“Before using a CT in our planning, we would look at pre-op studies, like a CT or MRI, and make our best guess as to what the correct position is during the surgery,” Dr. Tomlinson says. “Usually we could get pretty close, but for someone who does not do many replacements, this can be challenging.”

Knebel with wife Jayne
The new CT scans enable doctors to create a three-dimensional model of the shoulder, virtually place the implant into the model on a computer and adjust it until it is placed with exactness, based on the patient’s anatomy. This offers the surgeon a patient-specific plan for the procedure. The computer model is then used to create a physical 3D printed model of the patient’s shoulder with guides that attach during surgery, to ensure the implant is placed precisely in the right position.
Dr. Tomlinson has been using the 3D mapping for roughly three years, including on Knebel, who said he was completely pain-free after a week. By his six-week checkup, he had regained half of his range of motion. Three months after surgery, he had regained full mobility.
“By placing the shoulder in a more exact position, there’s better overall function,” Dr. Tomlinson says, adding that the biggest frontier now is “to make these shoulders last longer.”
Shoulder replacements can take up to a year to fully heal, although 90 percent of the recovery takes place in the first six months, says Dr. Tomlinson. And though Knebel continues to heal, he would recommend Dr. Tomlinson to anyone.
“I am in no pain or discomfort,” Knebel says. “I can do things with my arm and shoulder that I couldn’t do before. I am very happy I had this surgery done.”